Intricate Interplay Between the Gut Microbiome and Intestinal Immunity
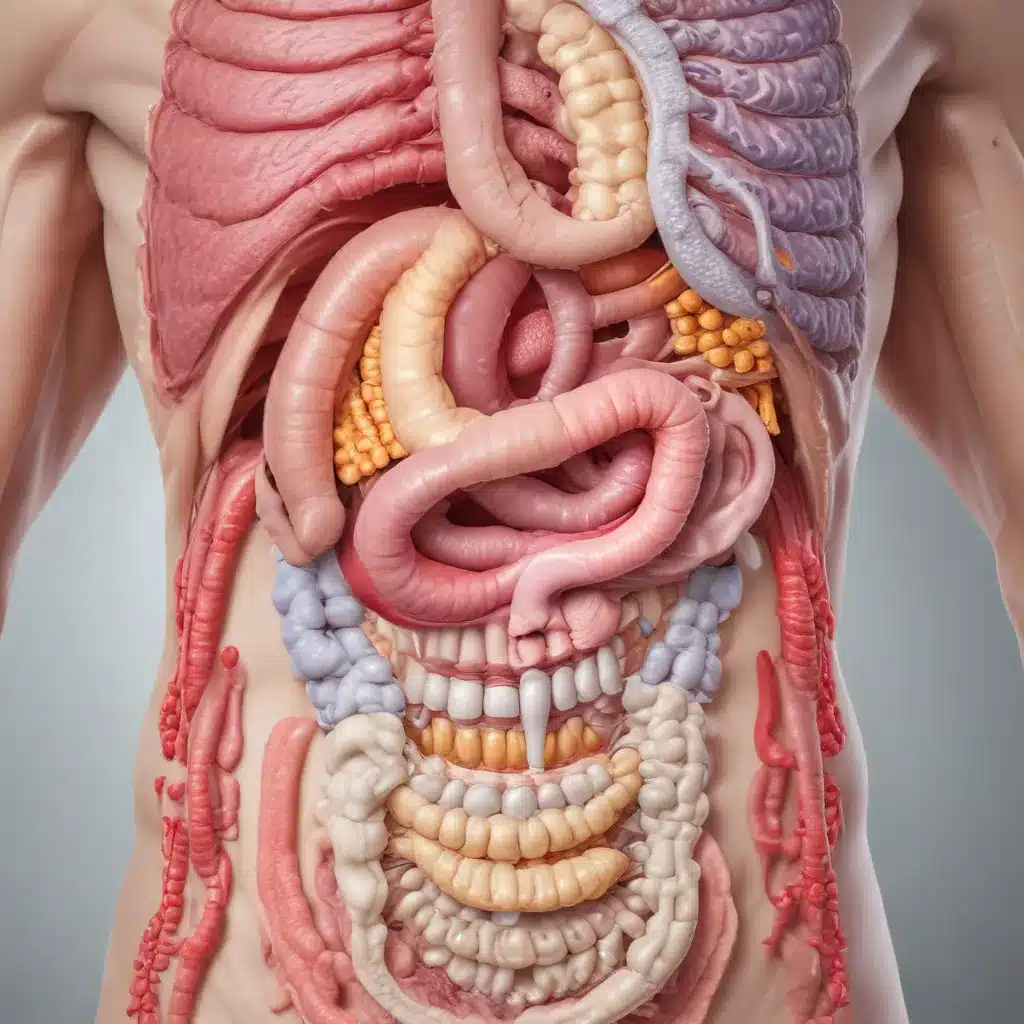
The human gut is home to a complex and dynamic microbial ecosystem, the gut microbiome, which plays a crucial role in maintaining intestinal homeostasis and overall human health. This diverse community of microorganisms, including bacteria, archaea, viruses, and fungi, exists in a delicate balance, interacting extensively with the host’s immune system.
Gut Microbiome and Intestinal Immune Development
Early-life colonization of the gut microbiome is a key driver of immune system maturation. The immaturity of the infant immune system renders newborns highly susceptible to infectious diseases. However, the microbiome’s establishment during this critical window can have long-lasting impacts on immune function and susceptibility to inflammatory and autoimmune disorders later in life.
Studies have shown that the absence of a diverse gut microbiome in germ-free animal models is associated with profound defects in the development and architecture of intestinal lymphoid tissues, as well as reduced populations of key immune cell types like intraepithelial lymphocytes and IgA-producing plasma cells. Colonization with specific commensal bacteria, such as segmented filamentous bacteria, can induce the differentiation of pro-inflammatory Th17 cells, while the polysaccharide A from Bacteroides fragilis promotes the maturation of the adaptive immune system.
Microbiome-Immune Crosstalk at the Intestinal Barrier
The best-studied interface for microbiome-host interactions is the intestinal mucosa, where the immune system must maintain a delicate balance – tolerating the vast numbers of commensal microbes while defending against pathogens. This is achieved through various mechanisms that compartmentalize the microbiota and prevent their incursion into the sterile body milieu.
The intestinal epithelium, comprising a single layer of specialized cells, forms a critical physical barrier that separates the gut lumen from the underlying tissues. Mucus secreted by goblet cells, antimicrobial peptides, secretory IgA, and tight junctions all work in concert to maintain this barrier function and restrict microbial access to the host.
Pattern recognition receptors like Toll-like receptors and NOD-like receptors on intestinal epithelial and immune cells recognize microbial signals, triggering signaling cascades that shape the microbiome composition and immune homeostasis. For example, the NLRP6 inflammasome regulates mucus secretion and microbiome configuration, while NOD2 controls the expression of antimicrobial peptides and restricts the growth of specific commensal bacteria.
Dysregulation of the Microbiome-Immunity Axis in Inflammatory Bowel Diseases
Inflammatory bowel diseases (IBD), including Crohn’s disease and ulcerative colitis, are chronic, relapsing disorders characterized by an aberrant immune response to the gut microbiome. Genetic and environmental factors that disrupt the delicate balance between the microbiome and the immune system are believed to play a central role in IBD pathogenesis.
Microbial Dysbiosis and Intestinal Barrier Dysfunction in IBD
Patients with IBD exhibit marked shifts in the composition and diversity of the gut microbiome, including decreased abundance of beneficial taxa like Bacteroidetes and Firmicutes, and increased prevalence of potentially pathogenic Proteobacteria. These microbial imbalances are often accompanied by impairments in the intestinal epithelial barrier, such as reduced mucus layer thickness, compromised tight junctions, and depletion of antimicrobial peptides.
The breakdown of the intestinal barrier allows for the translocation of commensal bacteria and their products, triggering an aberrant immune response that perpetuates intestinal inflammation. Genetic susceptibility factors, such as mutations in the NOD2 gene, can further exacerbate this dysregulation by impairing the host’s ability to maintain homeostasis with the gut microbiome.
Role of Innate and Adaptive Immunity in IBD
The intestinal immune system plays a central role in the pathogenesis of IBD. Innate immune sensors like TLRs and NLRs, which recognize microbial ligands, are dysregulated in IBD, leading to altered cytokine production, immune cell activation, and disruption of the intestinal barrier.
On the adaptive immune side, IBD is characterized by an imbalance between effector T cell responses, such as Th1 and Th17 cells, and regulatory T cells. This skewed T cell homeostasis, coupled with defects in B cell-mediated secretory IgA production, further exacerbates the inflammatory state and inability to maintain tolerance to the gut microbiome.
Emerging Therapeutic Strategies Targeting the Microbiome-Immunity Axis
Given the central role of the microbiome-immunity interplay in IBD pathogenesis, novel therapeutic approaches aim to restore this delicate balance through various interventions.
Fecal Microbiome Transplantation and Probiotics
Fecal microbiome transplantation (FMT), which involves the transfer of fecal material from a healthy donor to the patient, has shown promise in treating recurrent Clostridioides difficile infection. While the efficacy of FMT in IBD is still under investigation, the technique holds potential for reshaping the gut microbiome and reestablishing immune homeostasis.
Probiotic supplements, containing beneficial bacterial strains, have also been explored as a means of modulating the gut microbiome and immune function in IBD. Clinical trials have reported improvements in disease symptoms and markers of inflammation with the use of specific probiotic formulations, though the overall efficacy remains a topic of ongoing research.
Dietary and Microbial Metabolite-Based Interventions
Diet is a key environmental factor that shapes the gut microbiome composition and function. Dietary fiber, for instance, serves as a substrate for the production of anti-inflammatory short-chain fatty acids by commensal bacteria, which can strengthen the intestinal barrier and regulate immune responses.
Microbial metabolites, such as tryptophan-derived indoles and secondary bile acids, have also been investigated for their potential to influence intestinal immunity and maintain homeostasis. Targeting these microbial-host interactions through dietary or supplemental interventions represents a promising avenue for IBD management.
Challenges and Future Perspectives
While significant progress has been made in understanding the intricate relationship between the gut microbiome and the immune system, and its implications for IBD, many challenges remain. The high degree of individual variability in the gut microbiome composition, the complexity of microbial-host interactions, and the multifactorial nature of IBD pathogenesis present barriers to developing universally effective microbiome-based therapies.
Future research efforts should focus on integrating multi-omics data (metagenomics, transcriptomics, proteomics, metabolomics) to gain a more comprehensive understanding of the mechanisms underlying microbiome-immunity crosstalk in health and disease. Personalized approaches that account for individual variations in the gut microbiome and immune status may be necessary to unlock the full potential of microbiome-targeted interventions for IBD and other immune-mediated disorders.
Continued advancements in this field hold promise for the development of novel diagnostic biomarkers, tailored therapeutic strategies, and preventive measures that harness the power of the gut-microbiome-immune axis to improve the management of inflammatory bowel diseases.

